Case:
73 yo
male with PMH of CAD s/p CABG, hypertension, other medical history unavailable.
C/C sudden cardiac witnessed by his wife at approximately 10:55 am. CPR
instructions given to his wife over the phone by the 911 operator. Police
arrived minutes later to continue CPR with an AED. The BLS team arrived shortly
after and assisted with the resuscitation using an AED, BVM, OPA and supplemental
oxygen. ALS arrived 14 minutes after the 911; BLS reported 3 AED
defibrillations prior to ALS arrival.
Initial
ECG is coarse ventricular fibrillation and the patient was defibrillated at
360J by ALS. High-Quality CPR continued. Vascular access established with a right proximal humoral IO,
1mg of epinephrine given and repeated every 4 minutes during CPR. Paramedics
intubated the patient without an interruption in chest compressions; initial
EtCO2 is 40 mmHg. 2 minutes later, the patient is noted to be in
refractory VFIB despite serial defibrillations and anti-dysrhythmics. A total
of 14 defibrillations, amiodarone, magnesium and lidocaine were required to
convert the VFIB to an organized pulseless sinus ECG rhythm with a QRS width of
160 msec. The patient also received calcium and sodium bicarbonate. Return of
spontaneous circulation (ROSC) was noted 38 minutes into the resuscitation.
This patient received approximately 1200 cc of crystalloid IVF, atropine and
push dose pressors (1:100k Epi) to maintain hemodynamics during transfer to the
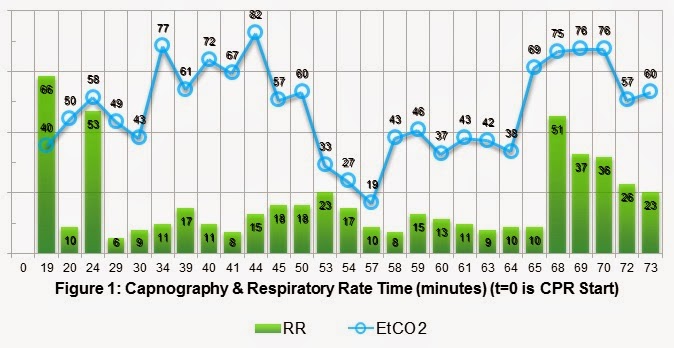
ED. Pulses were lost during
transport for 8 minutes and required CPR and additional epinephrine. Below is a
plot of his EtCO2 and respiratory rate versus time. ROSC#1 @ t=38 minutes and ROSC#2 at t=65 minutes.
Kodali and
colleagues recently published an excellent review of the usefulness of
capnography in Care of the Critically Ill and Injured. The literature search
was quite extensive looking at peer review papers from 1960 to 2014, covering
primary research, case reports and other review papers. Figure 2 is a summary
of the different clinical applications. Conformation of endotracheal intubation
is quoted in Kodali's paper as both 100% sensitive and specific, with 3 decades
of data for detecting correct tube placement. This has been known for a while
in EM and nice to repeat as often as possible because few tests have that level
of certainty. Waveform Capnography is the most definitive evidence of
correct endotracheal tube placement, thus eradicating the unrecognized
esophageal intubation.
Capnography
has been demonstrated to reflect the patient’s cardiac output (CO) during a
resuscitation based on the height of the waveform. The greater the CO the more
CO2 is off loaded in the lungs and measured on exhalation. Current Evidence demonstrate EtCO2 levels less than 10 mmHg
during chest compression is not likely to generate ROSC, so every effort should
be made to maximize the quality of CPR and treat reversible causes of arrest.
A certain
level of prognostication or prediction is also gained by the routine use of
capnography during CPR. Abrupt increases in EtCO2, generally a jump greater than 10-20 mmHg, is a marker of
ROSC, and, conversely, refractory EtCO2 values less than 10 mmHg has
identified 100% of patients who were unsuccessfully resuscitated. Kodali
found that the cumulative max EtCO2 > 20 mmHg at all time points
measured between 5 and 10 minutes post-intubation best predicted ROSC
(sensitivity of 88%, specificity 77%). EtCO2 is a valuable
tool in real-time decision-making during resuscitation.
Other
uses of capnography include monitoring of airway patency and respiratory rates.
The waveform capnograph and the ability to set warning alarms will instantly
alert providers to apneic conditions, such as obstruction or displacement. In
clinical situations where a patient is sedated or obtunded, EtCO2
will herald hypoventilation or apnea much sooner than traditional SpO2
monitoring.
Back to
our case, after reviewing figure #1, we can apply all the previously mentioned
key points to capnography. EtCO2 definitively confirmed ETT
placement. ROSC was predicted at t=10 minutes by an EtCO2 value
greater than 20 mmHg. High-Quality CPR was performed while reversible causes of
the arrest were managed. ETT patency was maintained throughout the encounter
and transfer to the ED. This would have been a great case to use 720 J Double
Sequential Defibrillation (DSD) for refractory ventricular fibrillation.
References:
1.
Goto,
Y; etal. “Termination-of-resuscitation rule for
emergency department physicians treating out-of-hospital cardiac arrest
patients: an observational cohort study”. Critical Care.
2013;17:R235.
2.
Kodali,
BS; etal. “Capnography during cardiopulmonary
resuscitation: Current evidence and future directions”.
J Emerg Trauma Shock. 2014;7(4):332-340.
3.
Meaney, PA; etal. “Cardiopulmonary
Resuscitation Quality: Improving Cardiac
Resuscitation Outcomes Both Inside and
Outside the Hospital. A Consensus Statement From the American Heart Association
Endorsed by the American College of Emergency Physicians and the Society of
Critical Care Medicine”. Circulation.
2013;128:417-435.
4.
Neumar, RW; etal. “Part 8: Adult Advanced
Cardiovascular Life Support: 2010 American Heart Association Guidelines for
Cardiopulmonary Resuscitation and Emergency Cardiovascular Care”. Circulation.
2010;122[suppl 3]:S729–S767.

No comments:
Post a Comment